Professor Cynda Hylton Rushton and Rheanna Hoffmann recently engaged in a moving video podcast conversation that highlighted the scars and distress of what it means to be a frontline nurse during the COVID pandemic. They covered not only the impact on nurses physical and mental health but also explored strategies that could be adopted by nurses to manage their distress. Cynda will be a key presenter at the free, online Healing Healthcare Summit in early February 2022.
Cynda is incredibly well-informed about nurses experiences during the pandemic, being a nurse herself and working with nurses to develop what she calls “moral resilience” – the ability of an individual to “restore or sustain” integrity in the face of the onslaught of challenges to their inner harmony and capacity to align their words and actions with their values and deep commitments.
Cynda, whose focus includes clinical ethics and contemplative practice, brings to the conversation penetrating insight and deep caring and compassion – characteristics that are manifested in her faculty work with the clinicians training program, Being with Dying. Cynda is the author of Moral Resilience: Transforming Moral Suffering in Healthcare.
Rheanna is an emergency nurse who is also a meditation practitioner and teacher with extensive experience in mindfulness and its benefits. During the worst of the pandemic in the US, she volunteered to work in New York City. Her personal recollections of this experience can be found in an interview where she shares an intimate insight into what happened for herself and others during the overwhelming crisis. Her presentation is part of the Mindful Healthcare Speaker Series which is readily available as a “resource for challenging times”.
In her discussion with Cynda, Rheanna provided an expose of her emergency nursing experience during COVID that is raw and vulnerable but manifests her openness and courage. I have previously reported on Rheanna’s interview about death and the dying process with Frank Ostaseski, Founder of the Zen Hospice Project. Rheanna herself is the Founder of The Whole Practitioner designed to help nurses “to rediscover health, balance and their core values” after experiencing burnout, exhaustion and deeply personal frustration.
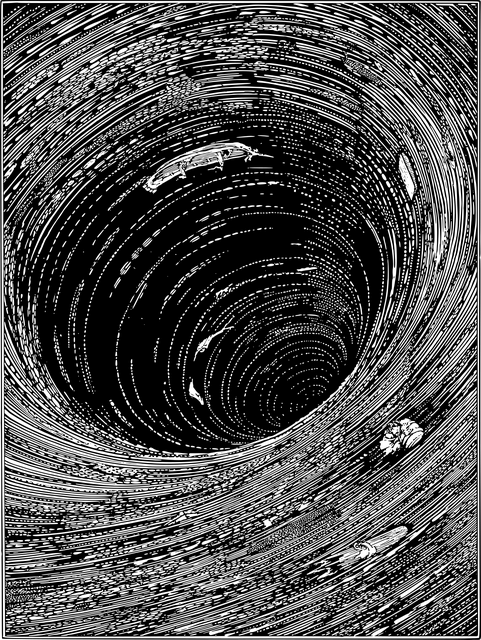
The distress of frontline COVID nurses
Rheanna recounted in telling detail the nature and extent of distress experienced by COVID nurses, especially those who were engaged in emergency wards. She spoke emotively about the following experiences and sensations:
- Reaching the limit of effectiveness of personal resources – whether that be yoga, friends or colleagues
- Experiencing isolation and loneliness – tendency to withdraw physically and mentally to deal with the overwhelm
- Feeling incredibly bare and vulnerable – the challenge of people dying and grief (that of relatives/friends and your own grief)
- Physical exhaustion – tired beyond belief and suffering from lack of sleep, resulting from replaying adverse incidences
- Feeling chronic hopelessness and helplessness – the challenges were beyond the capacity of individuals and the health system itself; exposure to personal limitations in the face of so much death and suffering. Associated with this sense of helplessness are nightmares, flashbacks, randomly crying and insomnia.
- Separation from self – the natural consequence of traumatic experiences.
- Loss of a sense of balance – impacting how time, health and relationships are valued or devalued (because of lack of time allocated to them)
- Burnout – on physical, psychological and moral levels. Rheanna described this as “acute burnout” reducing the energy for self-care and potentially leading to thoughts of suicide.
Rheanna pointed out that nurses, including herself, were normally able to “compartmentalise” their adverse experiences and do so in a way that was healthy, However, the adverse experiences from the pandemic were “unrelenting”, leading to chronic distress. Part of the frustration was the inability of frontline nurses to help others at times when they were feeling so “fragile”.
Self-caring strategies for frontline COVID nurses
Cynda offered several self-care strategies for COVID nurses during her conversation with Rheanna. Some covered ways of addressing negative self-talk while others focused on adopting a changed perspective and mindset or instituting a mindfulness practice:
- Mindfulness practice: Cynda offered a mindfulness practice that could be used by COVID nurses experiencing distress and burnout. This focused initially on the breath with the out-breath being viewed as a release of stress. In the exercise, the exhale stage was lengthened to accentuate and support release. Participants were encouraged to rest in the gap between the in-breath and out-breath and, where possible, extend this gap between breaths. A slow body scan was the next step with emphasis on identifying and releasing points of tension. Participants were encouraged to focus on an anchor of choice to stop their minds addressing their extended to-do list or diverting into worrying. Cynda suggested that nurse participants become conscious of how many miles their feet have travelled in pursuit of their daily caring and the level of support that their feet have provided. Lastly, she encouraged the nurses to employ statements such as:
- May I trust the wisdom of this moment consciously and fully.
- May I have the courage, honesty and openness to see things clearly and without judgment.
- May I be willing to let go of what impedes me rather than helps me.
- May I encounter a wise mentor to assist me to deal with these challenges.
- Confronting your own limitations: Rheanna pointed out the sense of guilt and shame that she experienced that were driven , in part, by her self-talk – “you could have done more”, “if only you had acted faster”, “if you had paid attention more fully you could have saved more people”, “if only you had been able to convince people to make different decisions”, etc. Our minds are very creative when it comes to self-denigration and negative self-evaluations. It is important to acknowledge that no one could have handled the challenges for nursing presented by the pandemic and not experience their debilitating effects. Cynda suggests that nurses need to “turn towards their limitations” and do so “with as much compassion “ as they extend to others. There is scope here for loving-kindness meditation for oneself.
- Changing your perspective: Cynda stated that the tendency in these crisis situations is to think that you are carrying the load by yourself because there is a natural tendency to turn inwards to cope with what is happening. She argues that what is required is a change in perspective. For example, she asked Rheanna to think about “Who else is carrying the load of the pandemic? “Who has your back? (e.g. friends, family, colleagues local and abroad & mentors).
- Separate effort from outcomes: Cynda maintained that a form of self-care is to acknowledge that the health outcomes are often beyond the control of a nurse. She stated that In her own work she does the best she can in the circumstances to meet an identified need but recognises that the specific outcomes are not in her control – there are too many intervening aspects impacting the final outcome. Cynda maintains that freeing yourself from expectations and outcomes is crucial for a nurses’ welfare. In the pandemic, COVID nurses such as Rheanna attempted to “fix unsolvable problems”. Nurses’ health outcomes were not the result of lack of effort or smarts but because the pandemic situation exceeded the capacity of individuals and the health system itself.
- Savour achievements – Cynda reinforces the view that the brain has a natural negative bias and is more likely to “mull over” what did not go well rather than “honour what we are able to do in the moment”, given the circumstances thrust upon us. She stated that nurses need to focus on how they made a difference in people’s lives, e.g., holding someone’s hands as they were dying, gasping for breath or having a tube inserted to enable them to breathe. This thought expressed kindly by Cynda precipitated a chain reaction from Rheanna who began to identify numerous moments when she “deeply showed up with people” and , in the process, rediscovered “what it means to be a nurse” and gained insight into the very core of her being and who she was. The other aspect that Rheanna savoured was her deep connection with people who were suffering – in spite of what was happening around her independently of her best efforts.
Reflection
Much of what Cynda proposed as strategies to help nurses deal with the extraordinary level of stress of frontline work during the pandemic can be incredibly useful for all of us to manage stress and resultant distress in our daily lives. As we grow in mindfulness through meditation, reflection and other mindfulness practices we can reshape our perspective and expectations, savour the positive in our lives (including being alive), confront our grief and limitations and achieve the freedom of separating outcomes from effort in our chosen endeavours.
___________________________________________
Image by Gerd Altmann from Pixabay
By Ron Passfield – Copyright (Creative Commons license, Attribution–Non Commercial–No Derivatives)
Disclosure: If you purchase a product through this site, I may earn a commission which will help to pay for the site, the associated Meetup group, and the resources to support the blog.