In the previous post, I discussed the ravages of Alzheimer’s disease on the mental. emotional and physical capacities of the affected person. I particularly emphasised the importance of self-care for the carer whose life is increasingly disrupted and made more stressful because of the cognitive, emotional and financial drain on their personal resources.
Alzheimer’s disease and the associated disorder of dementia are becoming increasingly prevalent in society as our populations age. The Alzheimer’s Association maintains that there are 342,000 people in Australia living with dementia and 44 million worldwide. The Harvard Medical School notes that Alzheimer’s disease is the major cause of dementia.
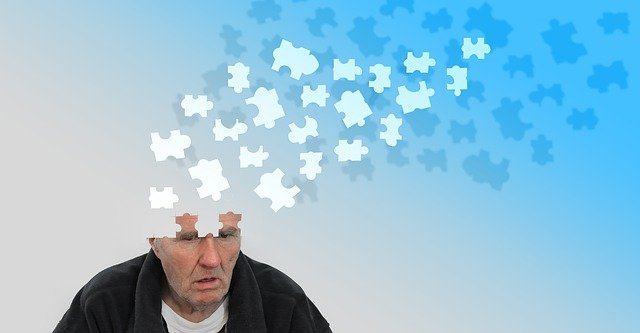
When you come into close contact with someone who is suffering from Alzheimer’s disease or other forms of dementia, you begin to realise the need to savour your brain as a source of wonder in everyday life. As you see the progressive loss of key faculties by another person, you begin to realise how much we rely on our brains to live effectively and happily in our day-to-day existence.
It is often only when we lose something, or see others lose something that we value, that we begin to really appreciate what we have. The same is true of our brains. And yet, as Andy Puddicombe points out in a YouTube video, we spend more time looking after our hair or car than we do our brains – the source of our thoughts, creativity, happiness, and practical skills. Andy suggests that all It takes is 10 mindful minutes each day to begin to mind our brains.
Protective measures
The Harvard Medical School, in their publication on Alzheimer’s disease and its treatment, suggest a range of protective measures that people can take to either avoid Alzheimer’s or to slow the progress of the disease. They point out however that scientists have not found a cure for Alzheimer’s or found definitive ways to prevent its occurrence – there are still many unknowns in relation to the disease, including the actual impact of genetic factors. The Harvard Medical School, however, notes that lifestyle factors are a major influence on preventing the disease or slowing its progress.
In line with many other sources such as the National Institute of Aging, the Harvard Medical School recommends exercise, diet, weight reduction, restful sleep and mental stimulation as protective measures. They remind us that what is good for our brain and body is also good for our heart.
The Harvard Medical School provides health reports on the benefits and techniques for different exercise routines. They particularly stress the multiple benefits of walking in their publication Walking for Health, including the positive impacts on blood pressure, memory, heart health and weight. Walking is one of the easiest and most accessible forms of exercise and they suggest that it is a good place to start for people who are not used to exercising. In a related article they identify 5 Surprising Benefits of Walking.
The recommendation re restful sleep accords with the research by Stanislas Dehaene, author of the book How We Learn: The New Science of Education and the Brain. Stanislas highlights the key role of sleep in consolidation of learning – in making our learning explicit and building “unconscious competence”.
Mental stimulation as a way to mind your brain
The Harvard Medical School maintains that while level of education has a positive effect on maintaining a healthy brain (through the process of creating “cognitive reserve” in the form of neurotransmitters and brain cells), what is more important as you age is to engage in activities that stimulate the brain. They suggest, like the Institute of Aging’s recommendations re “cognitive training”, that mentally stimulating activities such as playing music, reading, writing, doing puzzles and playing games, can help to develop and maintain a healthy brain despite physically ageing. There are many very active and inspiring octogenarians who provide testament to this possibility.
Minding your brain through mindfulness
Harvard Medical School, in the previously mentioned publication on Alzheimer’s, illustrates how this disease actually shrinks the physical brain as a result of the ”massive loss of brain cells” – which, in turn, “damages areas involved in thought, planning, memory, mood and behavior”. In contrast, Richard Davidson and Daniel Goleman in their book, Altered Traits: Science Reveals How Meditation Changes Your Mind, Brain and Body, reveal that mindfulness meditation actually increases the neo-cortex area of the brain.
They also contend that mindfulness meditation can shape your brain to build resilience. Drawing on the science of meditation they maintain that focused meditation and aligned action can develop the traits necessary for personal resilience – positive connections, awareness, insight into your inner landscape, clarity of purpose and a permeable self.
One of the positive effects of mindfulness meditation is better use and development of your working memory which is an area negatively impacted by Alzheimer’s disease. The act of paying attention facilitates short term memory thus enabling better retention and use of information for improved decision-making and behavioural choices. Harvard Medical School has a series of articles on improving your memory and a comprehensive report on how to keep your brain healthy in the face of age-related memory loss.
Specific mindfulness activities have particular effects relevant to minding your brain. Tai Chi, for example, enables you to deepen the mind-body connection as well as improve physical health, psychological well-being and overall energy levels (thus facilitating other forms of exercise such as walking).
Reflection
Harvard Medical School emphasises the need to mind your memory to offset the occurrence of memory lapses which are a natural part of the ageing process. Looking after our memory can be one of the many protective measures that we can employ to prevent or delay the onset of Alzheimer’s disease and its multiple debilitating effects.
As we grow in mindfulness, through meditation and other mindfulness practices such as Tai Chi, we can enhance our working memory, build resilience, develop our physical brain, and improve our overall psychological well-being which further reduces the strain on our brain brought on by life’s stressors. Developing the habit of mindfulness is a very sound and healthy resolution for the New Year.
___________________________________________
Image by Mabel Amber from Pixabay
By Ron Passfield – Copyright (Creative Commons license, Attribution–Non Commercial–No Derivatives)
Disclosure: If you purchase a product through this site, I may earn a commission which will help to pay for the site, the associated Meetup group and the resources to support the blog.