In the previous post, I discussed being mindful of mental health in the workplace. This involves not only awareness and being present to staff and colleagues, but also being able to recognise the early warning signs of mental illness and having the courage and competence to intervene.
The early warning signs of mental illness in the workplace
Recognition of the early warning signs of mental illness enables early intervention to prevent deterioration in a person’s mental health. Without such an intervention, issues can build up for the individual, making it more difficult for them to manage their stress and/or stressors.
The Mentally Healthy Workplaces Toolkit introduced in the earlier post provides a list of possible early warning signs of mental illness and lists them under five categories:
- Physical – such as constant tiredness, continuous ill health, major changes in appearance and/or weight, complaints about ongoing health concerns
- Emotional – such as irritability, loss of a sense of humour or of confidence, increased cynicism, nervousness, overly sensitive to perceived or real criticism
- Cognitive – overall performance decline through lots of mistakes, lack of concentration and/or inability to make decisions (constant procrastinating)
- Behavioural – behaving out of character by becoming more introverted or extroverted, withdrawing from group activities, lateness to work, not taking scheduled breaks (such as lunches) but taking unofficial time off
- In the business – inability to meet deadlines, declining motivation, frequent absences, working long hours unproductively.
There may be multiple causes for one or more of these early signs to occur. So, it becomes important to check in with the person involved as to how they are going and whether you can be of assistance.
Checking in – having the conversation
Often managers and colleagues are reluctant to say anything to the person showing early sings of mental illness and the person involved is often unwilling to raise the issue for fear of being seen as “not coping” or “being weak”. Part of the problem is that they really need support and care and genuine concern for their welfare. They can be experiencing a strong sense of isolation, lack of support and associated depression. Extending a helping hand can often work wonders. But how do you start the conversation?
People in the workplace are very ready to ask someone about a physical injury such as a broken wrist but when it comes to a mental illness they are often fearful or uncertain – yet the person with the early signs really needs someone to show care and concern. So, we can have a situation where the two parties – the manager/colleague and the person experiencing mental illness – are compounding the problem by not engaging in the conversation- a form of mutual withdrawal.
The recognised format for the initial conversation where someone is displaying the early signs of mental illness is called AYOK – “Are you okay?” The Mentally Healthy Workplaces Toolkit offers four steps for starting the conversation:
- Ask R U OK?
- Listen without judgment
- Encourage action
- Check in
It is useful to preface this conversation with the observation, “I have noticed that…and I am concerned for your welfare.” In other words, communicate what you have observed (shows you are interested in the person) and express care and concern.
The person involved may be unwilling to talk initially but it is important to undertake the occasional check-in. An experienced practitioner at the 19th International Mental Health Conference mentioned that on one occasion he had the initial AYOK conversation and the person involved said they were okay…and yet, some months later they came up to the practitioner and said, “I’m not okay, my daughter committed suicide three months ago – can you help me?” Having had the initial conversation opened the way for the subsequent voluntary disclosure. To avoid the conversation compounds the sense of isolation of the individual involved – they feel that they can’t help themselves and that no one else is willing to help them.
It is important to prepare for the conversation beforehand – know what you are going to say, allow time for the interaction and choose an appropriate time and place. You need to ensure that you are prepared to listen and be mindful during the conversation.
You can provide support by suggesting they use the Employee Assistance Program, visit their doctor (who can initiate a formal Mental Health Care Plan) or discuss options for making reasonable adjustments to their work situation. The important thing is that you take compassionate action, not letting the situation deteriorate.
It is vitally important to maintain confidentiality about any information disclosed to protect the privacy of the person involved. You will need the explicit consent of the individual to disclose the information to co-workers, for example. The information conveyed to you can only be used for the purpose intended by the disclosure – e.g. to enable a reasonable adjustment to their workload or pattern of work.
The exception would be where the person discloses that they are experiencing suicidal thoughts or feelings. In this case, you will need to seek professional support. Beyond Blue has some very sound and detailed guidelines for the conversation in these situations, including what language to use. ConNetica, in their blog post Chats for life APP, also provides an App (with practical conversation tips) which has been designed by young people for young people experiencing mental health problems, and possibly suicidal thoughts and feelings.
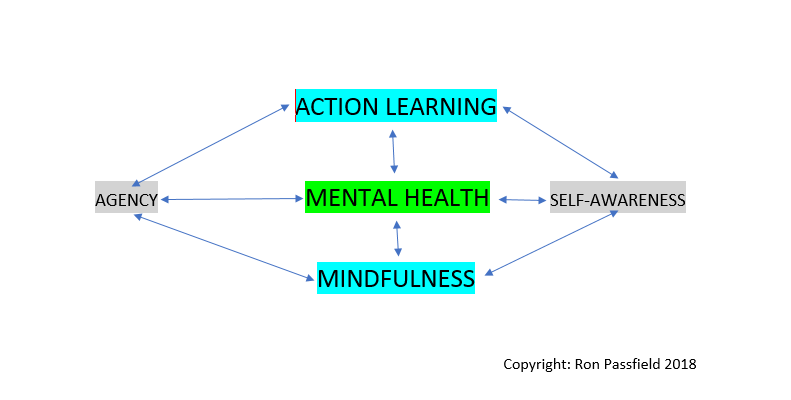
As we grow in mindfulness through meditation and reflection, we can become more aware of the early signs of mental illness, have the courage and confidence to have the AYOK conversation and a willingness to take compassionate action.
By Ron Passfield – Copyright (Creative Commons license, Attribution–Non Commercial–No Derivatives)
Image source: courtesy of geralt on Pixabay
Disclosure: If you purchase a product through this site, I may earn a commission which will help to pay for the site, the associated Meetup group and the resources to support the blog.