Self-care is often considered to be narcissistic or self-indulgent in a fast-paced world where we have multiple responsibilities and ever-changing demands. However, the reality is that in caring for ourself, protecting ourself from burnout, we are able to give time and energy from a place of abundance rather than from depletion.
In a previous post, I wrote about strategies suggested by various experts on how to manage ourselves in times of overwhelm. The focus in that article was on the overwhelm resulting from external events and circumstances as well as from our own health situation such as chronic illness.
In a talk given for UCLA Health, Diana Winston focused on the internal causes of “overwhelm”, namely, our own self-stories and patterns of thinking and doing. Her talk, Taking Care of Myself I Take Care of the World, focused on what we can do to redress the frenzied state of our lives as we endlessly pursue multiple conflicting goals. Diana stressed the need to prevent personal overwhelm, exhaustion and burnout and offered strategies for addressing this modern-day challenge.
The internal messaging that drives us
We might be caught up in activism over climate change, addressing issues of domestic violence or working to help redress the growing levels of homelessness. We might think that we must be doing something to help those in need and cannot rest until these needs are met. Diana cautious us that working in a frenzy is not going to enable us to make a “long-run, sustainable contribution”. She argues that if we are operating from “depletion”, we cannot give to the world in a “real and meaningful way”.
Diana quoted Thomas Merton who talks about self-violence when people over-commit in the face of conflicting demands. He argues that “frenzy” depletes our inner peace and “kills the root of wisdom that makes work fruitful”. This raises the question as to why we work in a frenzy when such a state destroys both the rewards and productivity of our work.
Diana suggests that sometimes this need to help everyone and “commit to too many people” comes from a sense of self-identity, needing to do something compassionate to feel validated. It might also be that it makes us “feel okay” if we are doing something to help others, we feel useful and not “empty” or useless. Diana acknowledged that in an early period of trying to help everybody all the time, she was working from a sense of feeling “not enough”, her inner voice was critical of her output.
Meditation and reflection to reverse frenzy
Thomas Merton argues that “we are so obsessed with doing that we have no time and no imagination left for being”. Diana maintains that we can recapture our sense of being-in-the-world through meditation and deep reflection. In the process we can unearth our negative patterns of thinking and gain clarity about the way forward for peace and productivity.
Diana argues for scheduling “a time of not-doing” in our diaries so that we can become less frenzied and less focused on doing. We can change our attitude from “running out of time” to expanding our time through delegation, asking for help and learning to act more productively and calmly by devoting some time to self-care. We can then contribute to the world through “overflow’, rather than depletion.
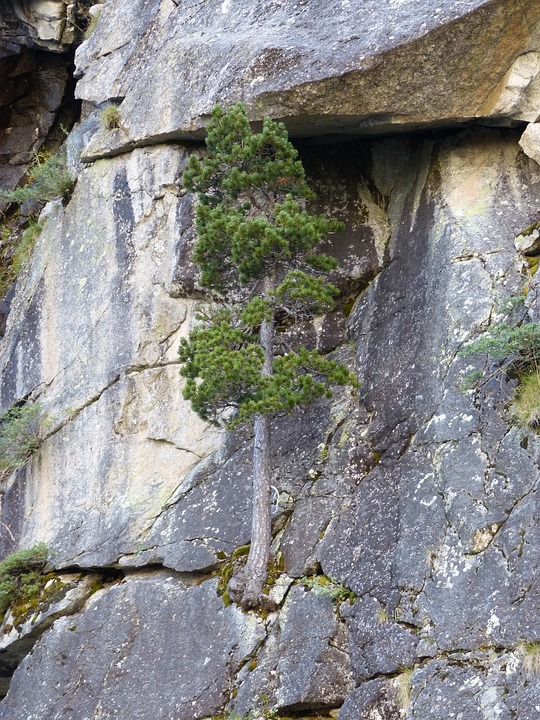
Diana also argues for the process of self-resourcing, building “positive states of mind” through pleasurable activities. This can involve forest bathing, meeting with friends, spending time in our garden, journalling, blogging, and engaging in compassion practices. We can imagine beautiful places that have brought us joy or revisit activities such as pickleball that offer enjoyment and fun. Tai Chi, meditation-in-motion, is another way to replenish our inner resources and develop our overall health and fitness.
When we don’t care for ourselves
When we get consumed by our work and frenzied activity we exhaust ourselves and operate from a state of depletion. Burnout, for example, causes depletion on the physical, mental and spiritual levels. We become tired and exhausted, overly negative and cynical and lose a sense of meaning in what we are doing.
Diana points out that we can’t give to others from this state of “emptiness”. Self-nurturing can rebuild “our bathtub” so that we can offer service and help from a state of “surplus” rather than deficit. When we are in deficit, every small challenge appears large and adds to our depletion. We become short-tempered, impatient and critical of others. So many things are seen to “stand in our way”.
Diana suggests that The Nap Bishop, Tricia Hersey, has a lot to offer through her focus on rest and relaxation. In her book, Rest Is Resistance, Tricia promotes the idea of napping, being prepared to say “no” and upholding personal boundaries as ways to “free yourself from the grind culture and reclaim your life”. She argues that in this approach lies true liberation and justice.
Reflection
When I think about self-care, what immediately comes to mind is my weekly glass of wine that I have to relax and wind down from the week. I rationalise this aberration from my diet on the grounds that it helps me focus away from work and is restful. However, with my chronic illness of MCAS, drinking alcohol is not self-care but self-harm. When I really reflect on what alcohol does to my body and mind, I have to ask myself, “Why do I persist in having my one glass a week when I know it is injurious to my health?”
As I grow in mindfulness through meditation, reflection and mindfulness practices, I can gain a greater insight into what drives my behaviour and develop the courage to create change so that self-care becomes a priority.
As part of this reflection, I wrote the following poem to help me unearth my thought patterns and reframe wine as self-harm, not self-care. Wine can no longer be viewed by me as a reward – it is a source of harm.
What is There About Alcohol?
What is the attraction?
like light to a moth.
It hurts my head,
makes my throat sore.
It damages my stomach,
strains my liver.
It aggravates my arthritis,
disturbs my sleep.
The pain outlasts the pleasure,
a mythical creation.
Is it for companionship?
Is it for conformity?
Is it for comfort?
Is it for control?
What do we see in this delusion,
where are the rewards?
_________________________________________
Image by Niels Zee from Pixabay
By Ron Passfield- Copyright (Creative Commons license, Attribution-Non-Commercial -No Derivatives.
Disclosure: If you purchase a product through this site, I may earn a commission which will help to pay for the site, the associated Meetup group and the resources to support the blog.